Introduction
If you want to understand where medicine is going, watch what happens when biology turns into data. Lung cancer is a brutal teacher, and in the last few years radiology has become a language that machines read with surprising fluency. The latest meta analysis pulls together 315 studies and makes a clear case. AI in oncology is not a toy. It already performs at a level that changes how we diagnose, stage, and plan care for real patients.
Table of Contents
1. Why This Study Matters
The hardest part of cancer care is not always the surgery or the drug. It is the uncertainty. Is this nodule malignant. How aggressive is it. Which patient will benefit from adjuvant therapy. The study at hand does not look at one model or one hospital. It aggregates hundreds of imaging studies for lung cancer, then reports pooled diagnostic accuracy and survival risk stratification. That scale shifts the conversation from anecdotes to evidence. AI in oncology moves from promising to actionable when the evidence is broad and consistent.
1.1 The Data Problem, And Why Imaging Helps
Pathology remains the gold standard, yet tissue is scarce, biopsies are invasive, and tumors change over time. Imaging sees the whole lesion and the surrounding tissue in a single session. Radiomics turns those pixels into thousands of quantitative features, then AI models connect those features to diagnosis and prognosis. This is not magic. It is measurement at scale, and it is exactly where AI in precision oncology earns its name.
2. What The Meta Analysis Actually Found

Here is the headline. For diagnosis on imaging, pooled sensitivity is 0.86, pooled specificity is 0.86, and the AUC is 0.92. For prognosis on imaging, pooled sensitivity is 0.83, pooled specificity is 0.83, with an AUC of 0.90. For survival risk stratification, patients flagged as high risk by AI models have more than double the hazard of death, a pooled hazard ratio of 2.53, and a similar boost in progression risk. In plain English, AI in oncology is good at finding cancer, it is also good at telling you who is in trouble.
2.1 Diagnostic Accuracy In Plain English
Imagine one hundred patients with suspicious nodules. With these pooled numbers, AI cancer detection will correctly flag about eighty six of the true cancers, and correctly reassure about eighty six of the non cancers. That is not perfect. It is clinically useful, especially when used as a second reader, a triage tool, or as a way to standardize thresholds across readers and scanners. The study also reports strong performance on tasks that matter for personalized cancer treatment, such as distinguishing invasive from pre invasive disease, classifying major lung cancer subtypes, and predicting EGFR mutation status.
2.2 Prognosis, Risk, And The Decisions That Follow
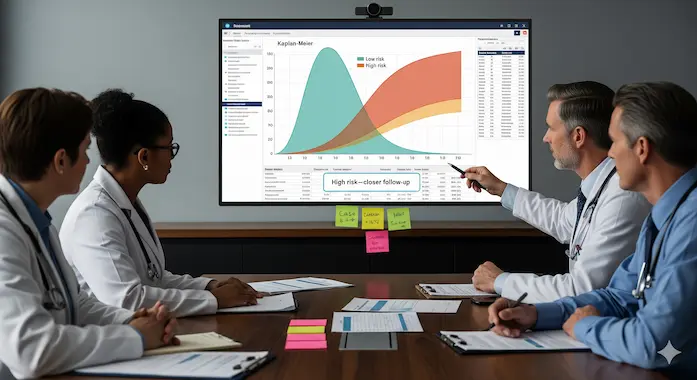
Prognosis is where many AI in cancer research claims go soft. This analysis holds up. Imaging based models can separate patients into higher and lower risk groups with clear survival differences. When the model calls a patient high risk, their overall survival hazard is about two and a half times higher than low risk. That separation allows oncologists to push for closer follow up, expanded staging, or earlier systemic therapy when it makes sense. It also delivers more confidence when the data says to hold.
3. A Quick Table You Can Bring To Tumor Board
Table 1 turns a dense paper into a single brief you can share with clinicians and data teams.
| Task | Metric | Pooled Result |
|---|---|---|
| Diagnosis on Imaging | Sensitivity | 0.86 |
| Specificity | 0.86 | |
| AUC | 0.92 | |
| Prognosis on Imaging | Sensitivity | 0.83 |
| Specificity | 0.83 | |
| AUC | 0.90 | |
| Survival Risk Stratification | Overall Survival HR, High vs Low Risk | 2.53 |
| Progression Free Survival HR, High vs Low Risk | 2.80 |
Numbers are pooled across multi study datasets. See study for subgroup details.
4. How The Machines See, Radiomics Meets Deep Learning
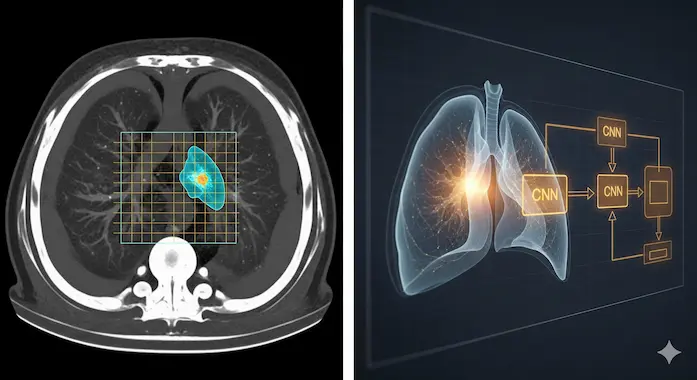
Radiomics starts with segmentation, then extracts hundreds to thousands of texture, shape, and intensity features. Classic machine learning models learn from those handcrafted features. Deep learning ingests the images directly and learns its own features. Both families perform well in AI medical imaging. In this analysis, deep learning edges out traditional approaches in several diagnostic and prognostic subgroup results, with 3D CNNs showing particularly strong diagnostic performance. That aligns with intuition. Tumors are three dimensional, and 3D models see what 2D cannot.
4.1 What Subgroup Analyses Tell Us
Two patterns matter for anyone deploying AI in oncology. First, internal validation usually looks better than external validation. Models dip when tested on independent cohorts, which is expected and healthy, and a sign to plan for distribution shift. Second, imaging only models often keep or exceed performance compared to models that naively mix imaging with scattered clinical variables. When you add data, add it well, or do not add it yet.
4.2 From Detection To Biology
The study goes beyond yes or no. Radiomics signals correlate with histology and with key molecular features like EGFR status. That opens the door to triaging molecular testing, guiding biopsy sites, and making first pass therapy decisions faster. It does not replace tissue. It focuses attention, saves time, and can reduce repeat procedures. That is the kind of practical leverage AI in precision oncology should aim for.
5. What This Means For Clinics, Engineers, And Patients
The diagnostic and prognostic performance is not the only story. The meta analysis also catalogues the habits of our field. Most studies are retrospective. Many lack true external validation. Heterogeneity is high. Publication bias exists. The authors call for prospective, multicenter trials and stronger reporting. That is the roadmap to reliable AI in oncology, and it is achievable if clinical and technical teams plan together from day one.
5.1 Build For Distribution Shift
If your model only looks good on your scanner and your radiologists, it is not ready. Train with realistic augmentation, then validate on clean, non augmented data from different sites. Expect performance to drop outside your walls, then design workflow that absorbs that drop. This is how AI in oncology moves from pilot to product.
5.2 Prefer Time To Event Modeling
Binary outcomes at six or twelve months hide the reality of survival data. Use Cox proportional hazards where possible. Report the number at risk, and publish curves with the detail needed for meta analysis. That kind of discipline pays off in the clinic, where decisions are rarely binary.
5.3 Treat Interpretability As A Requirement
Clinicians do not need a lecture on SHAP, they need a model that points to the region that mattered, and a probability they can use. Attention maps, transparent feature sets, and calibrated outputs improve trust and actionability. Good design here is not a luxury. It is part of patient safety. The study highlights interpretability as one reason adoption stalls. Build with that in mind.
6. Where AI Already Helps Today
Use AI cancer detection as a safety net for screening and follow up. Use AI in cancer prognosis to fast track high risk patients to tumor board and additional staging. Use radiomics cues to decide which nodules to biopsy first, and when to repeat imaging. None of this replaces the clinician. It extends their reach, and it makes the hard decisions a little less blind. That is the core promise of AI in oncology, practical gains that scale.
6.1 A Note On Scope And Claims
Lung cancer is heterogeneous. Subtype classification and EGFR prediction perform well in aggregate, yet molecular testing is still the standard for therapy selection. Keep AI in oncology grounded. Deploy where the evidence is strongest, measure carefully, and expand as prospective data arrives. Patients win when claims match data.
7. The Builder’s Checklist For The Next Twelve Months
- Define The Clinical Questions. Start with three tasks you can own in your setting, for example, nodule triage, invasive versus pre invasive classification, and survival risk grouping. Tie each to a specific action, not a scoreboard metric. This is the mindset that makes AI in oncology stick.
- Collect The Right Data. Curate imaging with consistent protocols, solid annotations, and enough diversity across scanners. Plan for an external validation set from the start. Publish both.
- Choose The Model Form Wisely. Use 3D CNNs when volume context matters. Consider radiomics plus machine learning when you need smaller, auditable models. Calibrate outputs.
- Design The Workflow. Decide where the model sits, triage, second read, or gate for additional testing. Decide who can override it and how. Build logging that a clinician can read.
- Ship Interpretability. Provide region highlights, case level explanations, and a probability the team can discuss in conference.
- Measure What Matters. Track changes in time to diagnosis, biopsy yield, and treatment initiation, not only AUC. Plan a prospective study or a registry. That is how AI in precision oncology earns trust.
The Bigger Picture, And A Clear CTA
If you are a clinician, ask for tools that bring these pooled gains into your workflow. If you are an engineer, build for external validation and interpretability, then prove it prospectively. If you are a hospital leader, back a pilot that measures patient centered outcomes, and publish the results. The evidence base for AI in oncology is already broad, with strong pooled accuracy in diagnosis and meaningful separation in survival risk. The fastest path to impact is simple. Pick one decision that matters, wire AI medical imaging into that decision, and make the outcome measurable. That is how AI in precision oncology becomes standard care, and how more patients see longer, better lives.
Source, Systematic review and meta analysis of artificial intelligence for image based lung cancer classification and prognostic evaluation, npj Precision Oncology, 2025.
1) What is the role of AI in cancer treatment and diagnosis?
AI in oncology reads medical images and other data to spot cancer earlier, classify disease, and predict how a patient will do. In lung cancer imaging, pooled results across 315 studies show diagnostic sensitivity 0.86, specificity 0.86, and AUC 0.92. For prognosis, AI separates high and low risk groups, overall survival hazard ratio 2.53. These tools guide screening, triage, and personalized cancer treatment.
2) How is AI being used in precision oncology today?
Clinics use AI for screening and AI medical imaging triage, lung nodule detection on CT, breast mammography worklists, and stroke or PE alerts. Researchers use AI to predict mutations and outcomes from scans and pathology, integrate multi-omics, and support trial selection. National Cancer Institute resources and FDA-cleared imaging AI catalogs show rapid growth across these use cases.
3) Can AI detect cancer more accurately than a human doctor?
In some settings, yes, especially when AI supports clinicians. Large prospective screening studies report higher detection with similar or lower recall, for example a German program saw a 17.6 percent increase in detection with AI-supported double reading. A Swedish randomized trial reported more cancers found and 44 percent less reading workload. Lung imaging AI shows strong aggregate accuracy, but best results come from AI plus experts.
4) Will AI replace oncologists?
No. Evidence and real-world adoption point to AI as an assistant, not a replacement. Radiology and oncology use AI to prioritize urgent cases, standardize reads, and save time, while clinicians remain accountable for diagnosis and treatment decisions. Health systems report rising AI use with hundreds of FDA-cleared tools, yet oversight and workflow fit still require human expertise.
5) What is radiomics and how does it help in cancer prognosis?
Radiomics converts CT, MRI, or PET images into quantitative features that capture shape, texture, and heterogeneity. These features link to tumor biology and outcomes, enabling AI in cancer prognosis, for example predicting survival or treatment response. Authoritative reviews describe the workflow, segmentation to feature extraction to validated models, and show prognostic value across cancers including lung.